Daniel’s harrowing journey through the complexities of health insurance highlights a growing issue affecting many patients in the United States. After enduring severe and relentless pain for months, his physician recommended an MRI to diagnose the cause. However, the necessary test required prior authorization from his health insurer. When the insurer denied this request, it marked the beginning of a painful ordeal that would last over a year. Daniel suffered from debilitating pain, significant weight loss, suicidal depression, and a reliance on opioids, all of which were compounded by the challenges of navigating insurance appeals.
The struggles faced by Daniel are not isolated incidents; they are emblematic of a widespread problem within the healthcare system. According to a recent survey involving over 1,300 respondents, 36% reported encounters with coverage denials, often related to prior authorization requirements that delayed necessary medical care. This tactic, commonly utilized by private insurers, has been a source of frustration for both patients and healthcare providers alike. Despite the eventual approval of many prior authorizations, the delays in the approval process foster distrust and exacerbate anxiety concerning medical care.
Starting next year, Medicare beneficiaries will also find themselves contending with similar roadblocks. Under a new pilot program, the Centers for Medicare and Medicaid Services (CMS) plans to implement the Wasteful and Inappropriate Service Reduction (WISeR) Model, which introduces a prior authorization process for traditional Medicare recipients in six states. This program will utilize artificial intelligence to determine the necessity of medical care, mirroring practices already common among private insurers.
Previously, Medicare’s traditional fee-for-service plans rarely employed prior authorization, with restrictions only applying to durable medical equipment. In contrast, nearly all Medicare Advantage plans now impose prior authorization requirements. The anticipated changes not only threaten to introduce administrative hurdles for traditional Medicare beneficiaries but could also prolong or deny access to critical healthcare services.
The burdens associated with prior authorization affect patients disproportionately, particularly those from marginalized backgrounds. Research indicates that lower-income patients are less inclined to appeal denials, and individuals suffering from significant health challenges, including those from Black and Hispanic communities, are often less successful in appeals. This raises concerns about equality in healthcare access, as the burdens of navigating insurance processes can lead to rationed care.
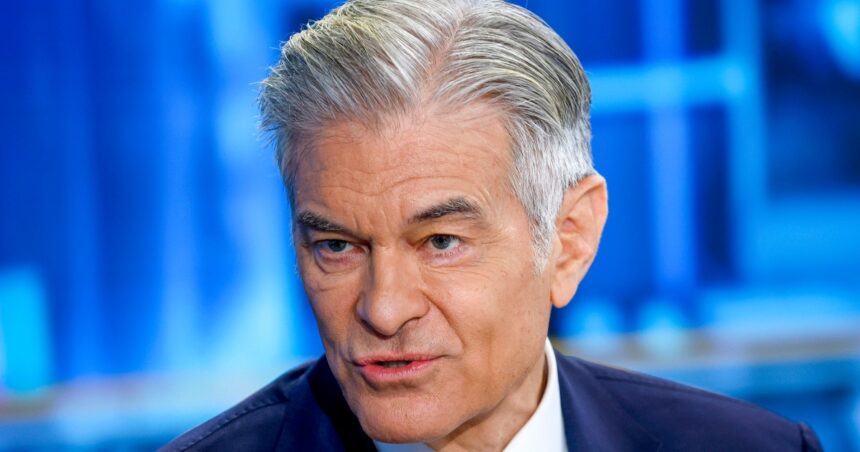
Dr. Mehmet Oz, CMS Director, contends that the intent behind the pilot program is to eradicate fraud and abuse within the system. Nevertheless, the reality may lead to increased delays and administrative burdens for healthcare providers and their patients. The difficulties in handling appeals and the complexities of coordination between physicians and insurers can create feelings of overwhelm, stripping patients of their sense of autonomy during vulnerable times.
Additionally, the dependence on AI for decision-making in healthcare claims has faced legal scrutiny. Lawsuits against major insurers challenge the use of AI, arguing that such systems often disregard the recommendations of treating physicians in determining coverage. The stress and burden of appealing denials dissuade many patients from challenging decisions, allowing insurers to maintain high rates of denial without significant repercussions—a calculated risk given the prevalence of successful appeals.
Ultimately, Daniel did receive the spinal cord stimulator he needed thanks to the advocacy of his family and supportive physicians who guided him through the insurance labyrinth. However, his experience underscores a larger systemic issue in a nation with ample resources. As the healthcare landscape evolves, particularly for vulnerable seniors facing cognitive and physical challenges, the pressing question remains: will patients continue to navigate a system entangled in red tape, risking their health in the process?